When Ebola ripped through communities in West Africa between 2014 and 2016, Tolbert Nyenswah saw at first hand how health workers extinguished the epidemic by finding and quarantining contacts of those who caught the disease. The former director of Liberia’s public-health institute thought contact-tracers would again rise to the challenge this year, keeping COVID-19 in check as it swept the globe. “Contact-tracing is one of the greatest tools that countries should deploy and use effectively to contain the outbreak,” he says.
But nine months after the World Health Organization (WHO) declared COVID-19 a pandemic, few countries are wielding contact-tracing effectively. “By now, what I was expecting is that 100% of people coming in contact with COVID-19 would have been traced,” says Nyenswah, now an infectious-diseases researcher at Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland.
Across the Western world, countries have floundered with this most basic public-health procedure. In England, tracers fail to get in touch with one in eight people who test positive for COVID-19; 18% of those who are reached provide no details for close contacts. In some regions of the United States, more than half of people who test positive provide no details of contacts when asked. These statistics come not from the first wave of COVID-19, but from November, long after initial lockdowns gave countries time to develop better contact-tracing systems.
The reasons for the failures are complex and systemic. Antiquated technology and underfunded health-care systems have proved ill-equipped to respond. Wealthy nations have struggled to hire enough contact-tracers, marshal them efficiently or make sure that people do self-isolate when infected or that they quarantine when a close contact has the disease. And overstretched contact-tracers have been met with distrust by people wary both of health authorities and of the technologies being deployed to fight the pandemic. Meanwhile, researchers who are keen to draw lessons from contact-tracing operations are stymied by a dearth of data.
A handful of places stand out as exemplars of successful contact-tracing — including South Korea, Vietnam, Japan and Taiwan. Many of these have cracked down on COVID-19 early, isolated infected people and their contacts and used personal data such as mobile-phone signals to track obedience. Not all of those techniques are transferable to countries now struggling to contain massive outbreaks. But they still provide some lessons.
Measures that work include tracing multiple layers of contacts, investigating outbreak clusters and providing people who are advised to quarantine with safe places to do so and with financial compensation. Technology might help, too: from software that streamlines conventional contact-tracing efforts, to smartphone apps that alert people that they might have been exposed to SARS-CoV-2.
A string of failures
The textbook version of contact-tracing starts with someone testing positive for COVID-19 and isolating themselves. A contact-tracer interviews this person to find out who they might have exposed while infected, usually from 48 hours before the positive test, or before symptoms appeared (if there were any). Close contacts — those who’ve spent more than 15 minutes close to the infected person — are of special interest, but anyone who shared public transport or an office space might qualify. Tracers then call or visit those contacts to tell them they need to quarantine, so that they don’t pass the virus on to more people. The chain of transmission is broken.
In reality, failures occur at every stage of this test–trace–isolate sequence. People get COVID-19 and don’t know it, or delay getting tested. Positive results can take days to be confirmed. Not everyone who tests positive isolates when requested; one survey in May found that in the United Kingdom, 61% of people who were self-isolating said they’d left their house in the past day1. People can’t always be reached for an interview or don’t provide details of their close contacts. And not all contacts are reached, or are willing to comply with quarantine orders.
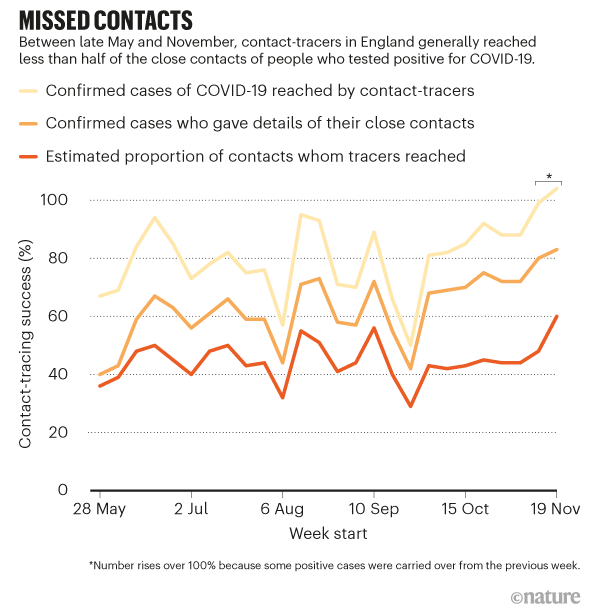
Because of this series of problems, researchers estimate that in England this year, tracers typically reached less than half of the close contacts of people who’d had a positive COVID-19 test (see ‘Missed contacts’). There are no data on how many of these contacts actually quarantined in turn.
The United States is in a particularly dire situation. “Public-health authorities are struggling to reach cases and contacts” despite aggressive efforts, says John Oeltmann, head of contact-tracing assessment at the US Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia. He and his team evaluated two counties in North Carolina. In June and July, 48% of cases in one county and 35% in the other reported no contacts. Of the contacts whose details were provided, one-quarter in one county and almost half in the other couldn’t be reached on the phone after three attempts over consecutive days2. In New Jersey, just 49% of cases between July and November were contacted; only 31% of those provided any contact details. “These results are not rare,” says Oeltmann.
Such data, which demonstrate how poorly contact-tracing is working, are scarce. Only a handful of US states openly report contact-tracing metrics. And although the European Centre for Disease Prevention and Control (ECDC) lists the types of data that countries should gather to monitor contact-tracing efforts, none is reported back to the ECDC or is readily available for comparison. This makes it difficult to compare failures in contact-tracing between countries.
Finding contacts
In South Korea, authorities use data-surveillance techniques to get around the problem of people being unwilling to disclose — or unable to recall — close contacts3. “We need to double-check,” says Daejoong Lee at the South Korean Ministry of Economy and Finance. A law passed in response to an outbreak of Middle East respiratory syndrome (MERS) in 2015 allows authorities to use data from credit cards, mobile phones and closed-circuit television to trace a person’s movements and identify others they might have exposed to the virus. Information about cases is published online, an approach that allowed the country to avoid broad lockdowns and “worked very well”, says Lee. Still, in March, the Korea Centers for Disease Control issued guidelines limiting the release of ‘excessive’ information, after regional governments published maps of infected people’s routes in too much detail. In one case, a person was wrongly accused of having an affair with his sister-in-law because their overlapping maps revealed they dined together at a restaurant.
Tracers in Vietnam also use extra data — such as Facebook or Instagram posts and mobile-phone location data — to check a person’s movements against those reported to contact-tracers. But the country’s success was down to “the boots on the ground”, says Todd Pollack, an infectious-disease specialist at the Partnership for Health Advancement in Vietnam, a collaboration that provides training and support for the nation’s health system. Contact-tracers interview people face-to-face and use the extra surveillance data to prod for more details. Other places, including Israel, Armenia, Russia, Ecuador and Taiwan, gather mobile-phone location data to aid contact-tracing efforts. But in Slovakia, a constitutional court suspended the government’s attempt to permit this practice.
Once tracers in Vietnam identify close contacts, they send them to designated quarantine facilities. It’s a practice that has worked elsewhere — including in Taiwan. Since August, the WHO has recommended this approach for suspected and confirmed cases, as well as for close contacts of cases, particularly if an infected person is unable to isolate themselves from others in their household4. Hong Kong and South Africa have non-mandatory quarantine facilities for close contacts, and others have facilities for travellers from abroad, but most countries lack out-of-home quarantine. In the United States, it’s estimated that one in five households lacks the space required to keep others in the house safe5.
Against the clock
The WHO’s benchmark for a successful COVID-19 contact-tracing operation is to trace and quarantine 80% of close contacts within 3 days of a case being confirmed — a goal few countries achieve.
But even that’s not quick enough, says Christophe Fraser, a mathematical biologist at the University of Oxford, UK. Transmission is too rapid and the virus can spread before symptoms emerge, he points out. Modelling by Fraser and his team suggests that even if all cases isolate and all contacts are found and quarantined within three days, the epidemic will continue to grow. He says that in a single day, 70% of cases need to isolate and 70% of contacts need to be traced and quarantined for the outbreak to slow (defined as each infected person passing the virus to fewer than one other, on average)6.
But there are ways that contact-tracers can get ahead of a rapidly spreading outbreak. One is to cast a wider net around each case, so that second-order contacts — ‘contacts of contacts’ — are traced and quarantined; in Vietnam, tracers sometimes reached out to third-order contacts if a case was identified late in its infectious cycle. As many as 200 contacts for each case are found and tested, says Pham Quang Thai, an epidemiologist at the National Institute of Hygiene and Epidemiology in Hanoi, who leads the national contact-tracing taskforce. “If we want to run as fast as the virus, we have to chase not only the first round,” he says.
“Tracing the contacts of contacts is a great strategy,” says Nyenswah. But in many places, he says, even tracing the first ring of contacts is proving tough.
The number of contacts identified for each COVID-19 case varies wildly, from an average of 17 per case in Taiwan, to 2 in the United Kingdom, 1.4 in France and less than one in parts of the United States. During the outbreak of severe acute respiratory syndrome (SARS) in Toronto in 2003, around 23,000 contacts for an estimated 251 cases — nearly 100 contacts per case — were told to quarantine. But it’s difficult to interpret these numbers. A country with no restrictions on movement will inevitably need to trace more contacts than one that is in some form of lockdown, for instance.
Another useful strategy is to trace a new case’s contacts as far back as a fortnight before they caught the virus, to identify who infected them. This ‘backwards contact tracing’ is extremely effective for the coronavirus because of its propensity to be passed on in superspreading events, says Adam Kucharski, an infectious-diseases modeller at the London School of Hygiene & Tropical Medicine. One study in Hong Kong found that 19% of cases of COVID-19 were responsible for 80% of transmission, and 69% of cases didn’t transmit the virus to anyone7. (The SARS outbreak in 2003 had similar transmission dynamics.) Any new case is more likely to have emerged from a cluster of infections than from one individual, so there’s value in going backwards to find out who else was linked to that cluster. Japan recognized this feature early and adopted cluster-focused contact-tracing in February; it traces contacts up to 14 days before symptom onset, rather than the usual 48 hours.
In Australia, contact-tracing lessons have been learnt the hard way. A second wave of COVID-19 cases sent the country’s second-largest city of Melbourne into a marathon lockdown in August that lasted for 112 days. By the time restrictions eased at the end of October, contact-tracers had adopted the Japanese practice of backwards-tracing contacts for the previous 14 days, and the Vietnamese practice of quarantining first- and second-order contacts. The overhauled system is yet to be tested, because the lockdown eliminated community transmission.
An army of tracers
All of these approaches require an army of contact-tracers, but few affluent Western countries had such people in reserve when COVID-19 hit, perhaps because outbreaks of infectious diseases are less common in those regions. In April, a US report (see go.nature.com/348knvz) estimated that around 30 contact-tracers per 100,000 people are needed during surges in case numbers — a nationwide workforce of nearly 100,000. At the time, the United States had only 2,200 contact-tracers. It now has around 50,000, but this ranges from 60 per 100,000 in Washington DC to 2 per 100,000 in Montana and Iowa. Vietnam had more than 12,000 trained contact-tracers at the outset.
Many regions have bolstered tracing efforts using students, off-work airline staff and volunteers, but have still struggled as case numbers rise. Germany planned to recruit to the level of 25 per 100,000, but imposed a second lockdown. So, too, did England, which has a tracing workforce close to 32 per 100,000. In countries that got on top of their outbreaks quickly, that level of workforce expansion was never required. Taiwan’s population of 24 million was served by 600 contact-tracers at the peak of its outbreak — just 2.5 contact-tracers per 100,0008.
Edward Salsberg, a health-workforce economist at George Washington University in Washington DC, says that a national or regional workforce could service different communities as hotspots occur. Private call-centre contractors are another workaround, but this strategy has mixed results. Outsourcing worked well in Massachusetts, says Marcus Plescia, the chief medical officer at the US non-profit Association of State and Territorial Health Officials, in Charlotte, North Carolina. But in England, poor coordination between contractors and health authorities left call-centre staff underused despite huge demand, according to media reports. Selina Rajan, a public-health specialist at the London School of Hygiene & Tropical Medicine, says that the quality of information also suffered. “It’s focused very much on the supply of people to make calls and not necessarily on the outcome,” she says. “I don’t actually think those people are really qualified enough.”
In the United States, public-health officials are faced with tough choices as tracers struggle to keep up. Some are prioritizing at-risk groups, or are ceasing to check on people asked to quarantine. The CDC now recommends that tracers focus on cases infected in the past six days, and encourages cases to notify their own household contacts. In California and New Mexico, lockdowns have returned.
Large swathes of the world now have widespread community transmission, meaning that numerous cases can’t be linked to identified ones — a sign that contact-tracing is failing to keep pace. In Vietnam, by contrast, “less than 1%” of cases during the latest outbreak had an unknown source, says Thai. These cases prompted a swift response, usually in the form of a hyper-local lockdown — of a single street, village or suburb — to contain the outbreak. Vietnam “just did everything you’re supposed to do”, says Pollack. Responders acted more quickly and maybe more comprehensively, he adds, “but it’s not like they did something magical”.
Still, high case numbers aren’t an excuse to give up on contact-tracing, Rajan says. UK government science advisers have been criticized for saying in February that the practice “should be discontinued” when cases got too high — advice the government followed in March — rather than urging the country to build up its tracing capacity. Abandoning contact-tracing left epidemiologists blind to details about where and why new cases were cropping up, Rajan says.
Technology tricks — and troubles
Smart data-management systems can ease the workload of contact-tracers and help countries get by with fewer disease detectives. Many nations, including South Korea, Vietnam and Germany, developed their own; state governments in Australia and the United States are adopting a commercial system. These are useful because they can record who has been contacted and avoid repeated phoning of people who are contacts of multiple cases, says Karin Verspoor, a computational linguistics researcher at the University of Melbourne — a situation that has been a problem in the United Kingdom and Australia.
Other tasks typically managed by contact-tracers can also be delegated to technology. In Vietnam, contacts log their health status through a symptom-tracking app, freeing up contact-tracers to interview newly infected individuals. People can also report the movements or symptoms of relatives who might not own a smartphone. In South Korea, Kenya and South Africa, authorities use phone location data to identify quarantine breaches.
At the beginning of the pandemic, overstretched contact-tracers in the United States, Australia and the United Kingdom faced the extra burden of antiquated health-care systems. In Australia, as well as in US states such as Hawaii and Washington, health departments are often notified of new cases by fax or phone. “It’s somewhat embarrassing,” says Plescia, but “we never invested in the systems to allow them to do it differently”. Entering names and other details into a database from faxed notifications causes big delays, he says, so that the window during which contact-tracing might make a difference vanishes.
“If there’s a single lesson that every country needs to learn, it’s invest in your public-health system,” says Rajan.
Assistance from apps
One idea touted early on was to do contact-tracing with smartphone apps. These emit Bluetooth signals to other phones; when a person tests positive for coronavirus, their phone app notifies others who were in close proximity for 15 minutes or more (if they have installed the app). In theory, such technology could notify contacts almost instantaneously. Apps can also help shop owners and restaurants to log who has visited their premises.
Contact-tracing apps have met with concerns over privacy, and although they are becoming common — at least 46 countries have developed some form of app — uptake rates remain low. “Adoption is not phenomenal anywhere,” says Effy Vayena, a bioethicist at the Swiss Federal Institute of Technology in Zurich, who is involved in the development of the Swiss contact-tracing app. “The trust question is crucial,” she says. It is exacerbated by a history of large-scale data breaches and privacy scandals in digital technologies.
Despite the low uptake, Fraser says, apps are a worthwhile adjunct to manual efforts, because small effects can accumulate over time. “This isn’t a silver bullet,” he says, but “it’s not just a gimmick”, either.
Trust deficit
For contact-tracing to work, people with COVID-19 must be prepared to answer questions about their whereabouts, and they must isolate themselves from others while unwell. In many places, that’s not happening.
A survey of attitudes to contact-tracing across 19 countries in August found that nearly three-quarters of respondents would be willing to provide contact information9. But rates varied. In Vietnam, only 4% of participants said that they wouldn’t provide this information. In the United States and Germany, the proportion was 21%, and in France, it was 25%. Concerns around data privacy and tracking are partly to blame, says researcher Sarah Jones at Imperial College London, who co-led the survey. “Many health authorities and governments, especially in North America and Western Europe, may need to urgently improve public-health messaging to mitigate concerns about contact-tracing,” she says.
“Public trust in all sorts of institutions is declining,” says sociologist Robert Groves, former director of the US Census Bureau, who notes that this is especially the case in large urban areas where social cohesion has also declined. But the low numbers of people providing details of contacts or responding to calls from contact-tracers, while disappointing, are not surprising, says Mary Bassett, a public-health researcher at Harvard University in Cambridge, Massachusetts. Some communities that have been hardest hit by COVID-19 have a long-standing distrust of public-health authorities, she says. “For the African American community, there’s a history of malfeasance on the part of the public-health system,” she says, “and for the Latino community, there’s a problem of members of the community who are undocumented” — and fear deportation.
Systems are often hampered by a lack of support for people who fall ill or need to quarantine, too. Providing adequate financial compensation for personal hardship as a result of quarantine could shift people’s reluctance to comply. The prospect of being without income for two weeks — or losing a job entirely — is a big burden, says Plescia, and might explain people’s reluctance to provide details for their close contacts.
If Western countries are not prepared to enforce case isolation (as Singapore does), quarantine contacts separately (as happens in Vietnam) or adopt digital measures to identify people (as in South Korea), some might ask whether contact-tracing is up to the task of suppressing the spread of COVID-19 in these locations — even if nations get better at recursive and backwards tracing .
But Nyenswah isn’t writing it off. Even in the United States, he says, the practice could yet work to bring case numbers down. It will be difficult, but it’s essential for regional and national leaders to clearly communicate the importance of contact-tracing, he says. “There is no substitute for political leadership in an outbreak response.”
"some" - Google News
December 14, 2020 at 05:40PM
https://ift.tt/37izUlT
Why many countries failed at COVID contact-tracing — but some got it right - Nature.com
"some" - Google News
https://ift.tt/37fuoxP
Shoes Man Tutorial
Pos News Update
Meme Update
Korean Entertainment News
Japan News Update
Bagikan Berita Ini

















0 Response to "Why many countries failed at COVID contact-tracing — but some got it right - Nature.com"
Post a Comment